The Second Patient Led NHS Mental Health Protest. How Many More?
A transcript of my meeting with the clinical psychology lead, Rachael Collier, of Chorlton House, Manchester. I release this information publicly as it is important to understand my NHS challenges.
I held a protest yesterday at Chorlton House in Manchester, which is a part of Greater Manchester Mental Health. This is my second protest as a patient.
I eventually got a meeting again with Chorlton House, with Rachael Collier, who is the clinical service lead for the service.
I post this transcript in full, and in good faith. I want people to understand why I am fighting for better therapy access, and if you want to learn more about my story, you can read my memoir.
If you have any questions about anything what me, or Rachael discussed, feel free to pop it down as a comment.
Rachael:
I appreciate you went to Chorlton House today. I have spoken to the specialist psychotherapy service, and wanted to get back to you.
One of the issues we spoke about was about short-term therapy, and how that’s difficult for yourself in terms of trust, and this is counter-productive in some way due to the Complex Post-Traumatic Disorder in play. Medication wouldn’t resolve absolutely anything in one, and therapies can be quite holistic, I agree. We wouldn’t expect people to get better with one session, either.
Emily:
I self-harmed last night, I literally did this protest with a bloodied bandage around me. If there was ever a more of a cry for help, I think I’d be dead. I’ve tried everything, I’ve contacted PALS, the complaints team, the whole lot. I’ve contacted Tony Warne and he hasn’t gotten back to me. So many people agree on the street that this lack of access to therapy is ridiculous, and we need to do something about it.
The problem is, even if you give me therapy which I do need, there are other people who are struggling in the same way. It can’t be that I am getting meetings with senior management because I am a journalist.
I got threatened by one of your workers today for singing out in the public. That was curtailing the right to protest as it was a public road. You know, there is a right to protest, I checked Liberty International before embarking on this, and I would like an apology.
Rachael: Obviously yeah, there is a right to protest.
Emily: I don’t even want to protest, I want change.
Rachael: Yeah, maybe the issue was shouting at a worker.
Emily: [for extra context] They told me there were vulnerable people in the building, as if I wasn’t vulnerable as well.
This is ridiculous.
Rachael: We tend to respond with short-term therapy on the basis that it is a short-term therapy service as appropriate to the situation.
Emily:
My question is, and it is a serious question. I’m a victim of child abuse. Where are people like me supposed to go? This is a genuine question.
The service refuses to admit it has problems, and it needs sorting ASAP.
I am also not the only one.
I have spoken to so many people who have also been victims of child abuse, and guess what? They get a diagnosis of Borderline Personality Disorder, without the psychologists EVER touching their trauma. I’ve seen this first hand.
This needs to change!
Rachael: Of course, we work with many victims of child abuse in the service.
Emily: So why are so many people being failed by the system?
Rachael: I guess that, that’s not really a topic that I can speak about, when you say ‘failed by the system’…
Emily: Lingering, and languishing on waiting lists. And I’m not the only one.
Rachael:
I mean yeah, obviously we’d like to see people in a timely way. We would like for people to not wait for too long. Being not an emergency service, there can be barriers to that.
We’re working within the parameters we were commissioned. There are waiting lists for many reasons, there’s an enormous amount of people accessing.
Emily:
But it’s also about the lack of communication.
I recently went to Poland to see their national health service, the NFZ, and they do publish wait times and how many people are waiting. If the NHS can’t provide extra therapists due to the economic situation, at the very least the NHS could have the courtesy to say how the situation is.
Not just ignore me; when I went to Chorlton House today, I got told to complain to my GP.
I was like, do you really think I would be ssitting there with a placard if I didn’t exhaust all my options? And having to sit there, considering litigation.
Rachael:
Yeah. We obviously work with people who have experienced childhood abuses amongst other things of course, but it is within the parameters of what we can provide. I know that we spoke last time, and you made it very clear that short-term therapy doesn’t work in your case, and we spoke about commissioning extended services.
Unfortunately, that’s not something that we can do.
Emily: Because it’s “Trust Policy.”
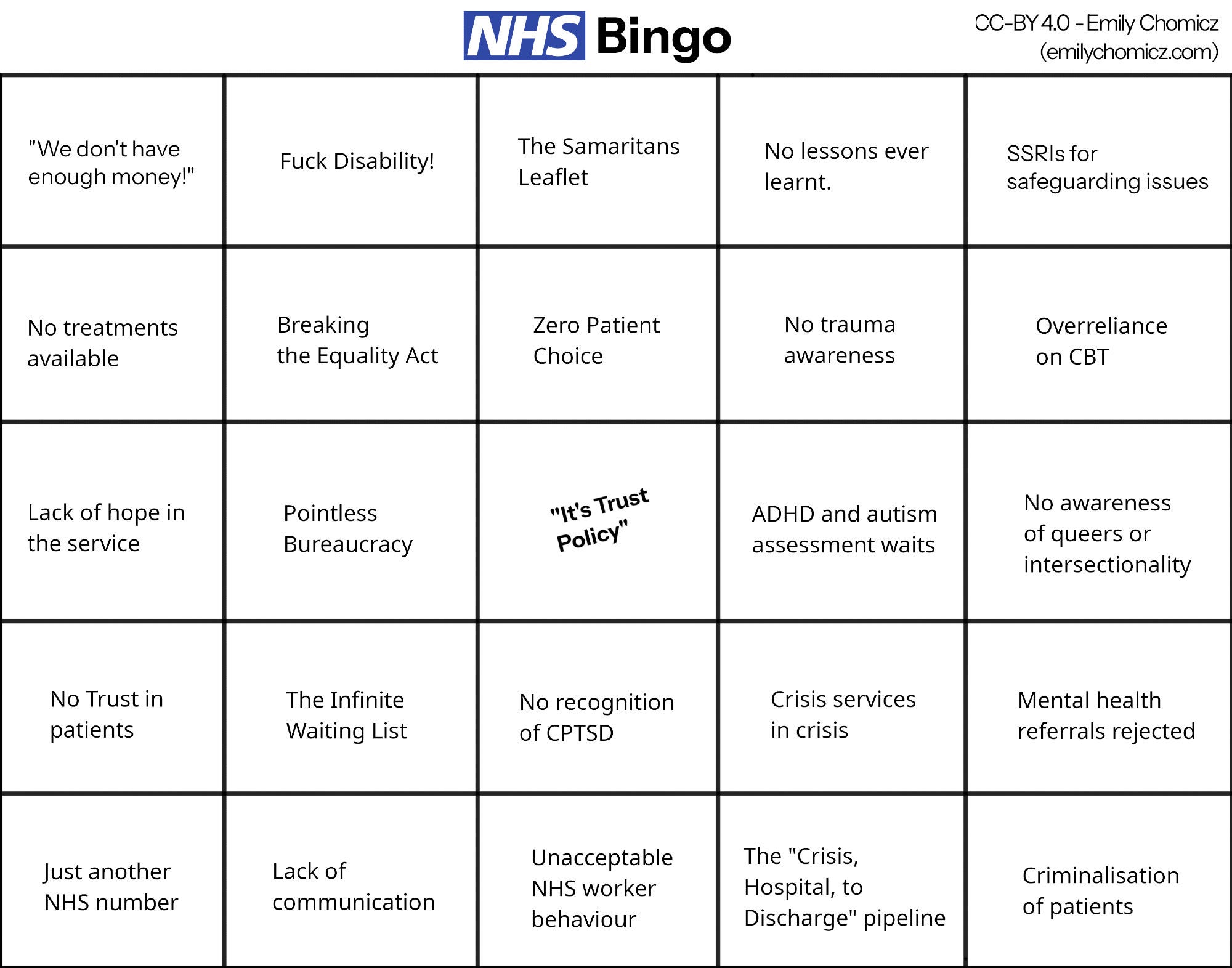
And God forbid anyone deviate from Trust policy. I literally have a bingo sheet in front of me, I’m ticking it off as we go. It’s ridiculous.
Rachael:
There’s a number of things, NICE guidelines say how many sessions are required for a lot of things – obviously it’s just a guide. And you said about the waiting list, and naturally, if we gave open ended courses of therapy to people, a) it wouldn’t be indicated in a lot of cases, you need to maintain a focus.
But b) it would prohibit people accessing therapy. We wouldn’t be able to pay for additional therapy outside what is provided.
Emily:
Why is it ‘equal treatment’ here, because not every patient is the same? That’s really important to understand. In the same way you wouldn’t leave a survivor of cancer with half of the cancer is still there. I don’t understand why it’s happening in mental health.
Rachael:
You’re right that not everybody is the same. When we’re working with people, it depends what the patient presentation is and what we focus on. I guess there will be different lengths of time that people need therapy, so some we will see less.
Emily
So, you can’t have a blanket solution of people get x amount of sessions because that’s not how it works at all in mental health. The problem in my case, maybe five years ago sure, sure, maybe the twenty sessions would have sufficed. But it’s been going on for so long, because I’ve not had treatment, I need more.
Rachael:
The specialist psychotherapy service should be for that, they are a slightly longer term service. They do an in-depth assessment, something like 3-6 sessions of assessment and formulation that can be helpful in itself, to get an understanding.
Emily:
Yeah, another waiting list. This is pointless bureaucracy, if you cut half of it out, there would be money, as the NHS has enough money, it just misspends it.
Rachael:
Yeah I guess that’s it really. I guess there are limits to funding certainly and the range of treatments for physical and mental health.
Emily:
Here’s the thing. I self-harmed last night, and I would have been entitled to go to A&E.
If I have self-harmed; let’s say, I don’t know what the actual costs are but say, an A&E attendance is £300, a therapist session is £60 a session privately.
That’s five sessions the NHS could have funded. That’s a waste of money. Going to A&E is expensive for the NHS and this bureaucracy is exactly why people end up in mental health crises in the A&E, and people don’t get help.
Rachael:
We do see a lot of people, and we do it within the premise of what we can offer and provide and that episodic care. But I can see that’s not right for you.
The NHS is a complex thing isn’t it, and it’s large organisation and can’t act in that nuanced way with hospitals, and talking therapy series acquainted in that way. It’s certainly not complementary is it?
Emily:
That’s why Greater Manchester Mental Health is rated inadequate by the Care Quality Commission. In other parts of the country, we don’t have this problem. This can’t go on.
This is how people will lose trust in the NHS, this is how politics will turn to the right, and abolish it because it doesn’t work. I am trying to help to fix the NHS. We are in a very precarious political situation.[discussions about co-production and asking to be signed up, again]
Rachael:
[personal details omitted regarding my specialist psychotherapist referral]
Emily:
Why does it take a meeting with you do to that? It really shouldn’t. It’s bizarre that I’m now having to go through a patchwork of systems, charities and other organisations because the NHS mental health system doesn’t work, it simply does not.
It doesn’t work when I get told to go to hospital, and then sit on the bloody waiting chairs for eight hours, and get told I’ll be referred, and then sent home again. Look at my medical records. It just doesn’t work. I got criminalised in one case for asking for help. I mean for crying out loud?
Rachael:
Have you sought assistance for that? Have you spoken to PALS?
Emily:
Yeah, still working on it. I’m too mentally ill to fight all fights. I have chronic pain issues, issues with my leg, and I cannot be expected to do this all by myself. This is a battle that I can’t fight alone. It seems that when I talk to the NHS, it feels like no lessons are ever learnt.
It’s all ‘I apologise’ and ‘we’ll refer you on to someone else’, and when I say, ‘I have been stuck in referrals for years’… I am told there would be another waiting list. This is Kafka’s Trial. Kafka would have loved to be alive to see this.
And also, if I get through to a therapist, and they’re unsuitable as they have been in the past, I get put on another waiting list. There’s no patient choice. Imagine a world where patients can choose their therapist privately, get funded by the NHS and this would be significantly cheaper for the NHS. Am I wrong?
Rachael:
I guess in an ideal world, we would be able to do this to a nuanced degree, but the reality is we should be providing a service for the wider population if you’d like. It can’t be so individualised.
Emily: Why not?
Rachael:
We can’t commission individually, we try and match and choose services that people want, and if people choose who they ultimately commission, and we do that for a large number of people, that becomes problematic.
Emily:
In the NHS constitution, it allows for a choice of patient care, when choosing a consultant, a hospital, or a GP, and most importantly the choice of the mental health provider.
If the NHS can’t provide a therapist, why don’t we do what the NHS has done for me in the past by providing NHS-funded private care for my physical health issues.
Rachael:
I do understand the frustration.
Emily:
The policy needs to change. The policy on commissioning needs to change. We’re commissioning stuff that doesn’t work for many people. The problem is, the NHS has now taken the route of giving CBT to everyone.
Is that appropriate though? No, people need different therapies. You can’t just give every individual computerised CBT, because people are not one-size-fit machines.
Rachael:
Some people find different approaches helpful, and we do have a range of treatments in line with NICE guidelines, but we don’t provide all treatments and that’s where the specialist psychotherapy service comes in as well.
Emily:
Why can’t my GP just refer me to that service in the first place then, and not be bounced around between Step 2, Step 3, and Step 3+? My GP felt pressured to prescribe me a mental health medication before the case can progress as the Community Mental Health Team (CMHT) requested this, and this medication sent me to hospital. It’s abominable. It’s ridiculous.
It’s ridiculous that I was under assessment for a CMHT and they couldn’t even diagnose OCD. What is the point of the service, if they couldn’t even diagnose a mental illness? My GP was not appropriately qualified to make a diagnosis, and had no input from Greater Manchester Mental Health.
Rachael:
It’s about treating the patient, not the individual disorders if you’d like.
Emily:
I have about eleven different mental health disorders, diagnosed, and I think it’s worth looking at them all, seeing what I was diagnosed with, and treating all of them. I was told by the Wythenshawe Hospital Home Treatment Team psychologist that the focus would be on trauma only.
There’s too many people involved, so we’re now just stuck in meetings which we are wasting public money on, as I, the patient, my friends, and loved ones have to suffer. The NHS’ inability to treat me means that everyone in the community suffers.
That is how you create a wider mental health crisis.
Rachael:
I think the psychologist shouldn’t have said that. With trauma of course, that affects people in a lot of different ways, and how you interact with others, and how you approach others. How we feel about ourselves and our sense of self and all sorts of things.
You can experience a whole lot of experiences, identity, and so on. Naturally, it’s about understanding all that together to some extent.
Emily: Will that happen in twenty sessions?
Rachael:
Yeah, and I guess the therapy service will try to have that in mind.
[more personal information shared regarding my referral]
Emily:
I’m tired of the culture in the NHS that the patient must be suspect just because they have trauma. Because that’s exactly what’s happening right now, there’s no trust in patients.
If I speak honestly about what I feel like, it goes in through one ear, and out the other. The patient knows themselves, they know what they need.
Rachael: Yeah.
Emily:
The culture of Greater Manchester Mental Health team is terrible. I have years ago been under the NHS Universities Greater Manchester Mental Health Team, I was under a psychiatrist.
A mental health nurse actually spoke up, and said, no, Emily shouldn’t be on all these medications for Bipolar II, but felt overruled by the psychiatrist.
It turns out I have cycle-related symptoms as I am a trans woman, and I’d like an apology. It’s not even about my referral anymore, it’s about what the hell is happening.
Patients get sidelined. We all know about the Edenfield Hospital scandal. It’s widespread.
Rachael:
Yeah, and that was obviously very shocking, wasn’t it?
Emily:
It’s not that shocking to me. And believe me, have spoken to a lot of patients that use Greater Manchester Mental Health’s services, because I used to run a mental health charity. This isn’t news.
Rachael:
These are questions I may not necessarily be able to answer, that’s more for leadership, and I’ll see what kind of forums there are for that for that.
Rachael:
Did you approach PALS? And what was the outcome of the email with Tony?
Emily:
Yes. I managed to get Tony Warne to reply to me on Bluesky as there was a missed email by the communications team.
I shouldn’t be expected to do this as a mentally ill person. Why am I having to contact the chair, Tony Warne, of the Greater Manchester Mental Health Trust, to get treatment and to stop this from happening?
It seems like common sense.
Rachael:
Mm. And what about your self-harm?
Emily:
I broke my ten year self-harm free streak. That should give you an idea of the level of my distress. I was so distressed last night, that I didn’t know what to do, so I self-harmed.I am now unable to go to hospital, as I have been unfairly banned from the hospital and I am in the process of disputing the ban. I can’t go to Manchester Royal Infirmary, because that’s too far and too expensive. None of my friends drive and are disabled. What am I supposed to do in distress?
I know crisis services exist in Manchester, like the Recovery Lounge and Bluesci@Night but they’re not therapists, they’re crisis workers. But the aim is this is surely for me to eventually stop needing them?
Because why am I having to use them still?
Rachael: [mm]
Emily:
Everything is overwhelming at this point. One thing builds on top of another. It’s the combination for everything.
[mm]
The first protest was me screaming out in agony, and that was me saying, I need help. I have had NHS clinicians today in my protest, see my sign briefly, and walk on.
That shows you the attitude and unacceptable behaviour of some clinicians as surely the right action would have been to ask if I was alright, not just walk on.
Rachael: [mm]
[I explain CPTSD to Rachael at this point]
Emily:
The NHS needs a specific pathway for child abuse, it needs to be built from scratch so patients like me can be treated at the right place, at the right time.
It reminds me of the state of women’s health and medical misogyny, when women get ignored by their GPs for period pains. I’ve seen this first hand. They could just investigate, and treat.
[conversation turns to managing my self-harm, and I went silent in response]
Emily:
The self-harm is a symptom. The thing about treating my self-harm is that the self-harm is a symptom, but not the cause. I’m fine. I have and will receive medical treatment.
But the big issue for me is that I should have ever, ever felt like that. Because it’s distressing not just for me, but people I live with.
Rachael: Have you tried plunging your face into cold water?
Emily:
I already know about that. I have read up on Dialectical Behaviour Therapy because of the waiting lists. I’ve basically become a defacto therapist myself by trying to manage my own symptoms without a medical professional. And I’m tired. I’m really tired.
Rachael:
I will let you know the outcome of the referrals and I’ll let you know if I get any more information, when it gets back to us.
Emily:
Just to let you know; at some point there may be a third protest and I will start litigation if this isn’t sorted, as I have suffered such extreme mental distress that the NHS has become a trauma of its own.
And that’s not acceptable from a health service.
Rachael: Mm. It sounds like you care very deeply about the wider mental health system.
Emily: Because I shouldn’t be an exception.
Rachael: Yeah.
Emily:
It’s not about caring, it’s about equality, and that’s important to me as a queer person, because it’s important to me.
It’s important that a secret handshake agreement isn’t made and I get therapy as long as I shut up. It’s important that I don’t get any special treatment here.
Rachael: Yeah. I think you started talking to Mark about that. It’s not about special treatment, it’s about making sure the mental health system is suitable for everyone.
[conversation comes to an end]